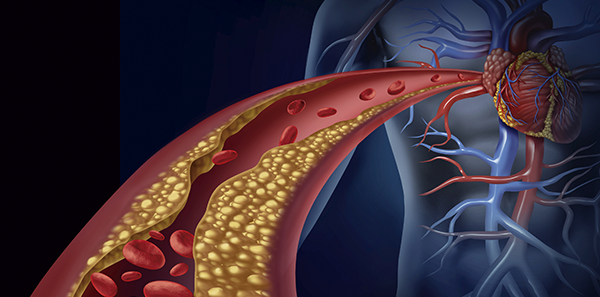
Inflammatory bowel disease (IBD) is a chronic inflammation of the intestine of unknown origin that progresses recurrently with flare-ups, some in which the disease remains active and others with remissions in which the symptoms disappear. It can present various complications and extra-digestive manifestations that accompany the intestinal symptoms, such as fatigue or weight loss.
The latest advances indicate that it’s caused by an excessive immune response that produces lesions of variable depth and extension in your body, but especially in the intestinal area.
Some of the factors that cause Inflammatory Bowel Disease include:
- Genetic predisposition and family history.
- State of the intestinal microbiota, also known as flora.
- Certain environmental factors, such as pollution.
- Exposure to certain micro-organisms.
- Abnormal immune response.
The concept of inflammatory bowel disease applies to two nosological manifestations, Ulcerative Colitis and Crohn’s disease. Both are characterised by being diseases which, as mentioned above, affect the intestine due to a fundamentally immune-mediated cause, presenting inflammatory and chronic problems that in some cases can cause life-threatening complications for the person affected.
- Ulcerative Colitis only affects the mucosa of the colon and rectum, which appears friable, that is, it disintegrates easily, and diffusely congestive. Its most frequent manifestations are:
- Diarrhoea.
- Presence of blood in the stool.
- Abdominal pain, fever and weight loss.
- Tenesmus, which is characterised by the constant urge to defecate even though the intestine is already empty.
- Perforation of the colon and even the risk of developing some types of cancer, are the most important risks to consider.
- In Crohn’s disease, the inflammatory process deeply affects the sub-mucosa and the other layers of the intestinal wall, with the presence of granulomas. It can affect any part of the intestines, even in other areas of the digestive tract. Its distribution is segmental, discontinuous, alternating inflamed areas with healthy areas of the intestine. Its most frequent clinical manifestations are:
- Diarrhoea – usually without the presence of bleeding.
- Abdominal pain, fever and weight loss.
- Fatigue.
- Fistulas, perforation or intestinal obstruction are the most severe complications.
Some of the available ways of diagnosing these diseases include blood, urine or stool analysis, abdominal imaging and endoscopic tests. In terms of the treatments that help to mitigate the symptoms or alleviate the disease, these include antibiotics, corticosteroids and immunomodulators that help to maintain the period of remission of the disease. However, it is important to note that no two diseases are the same, just as no two patients with inflammatory bowel disease are identical. This means there is no one single treatment for all patients and that diagnosis and treatment will be decided on by a physician based on the personal characteristics of each affected person.