Diagnosis is based on the correct diagnosis of angina pain, detection of ischemia (lack of blood flow) induced by various pharmaceutical drugs or proving the existence of obstructive coronary disease.
Diagnosis is obtained by looking at the relation between coronary pain and physical exercise.
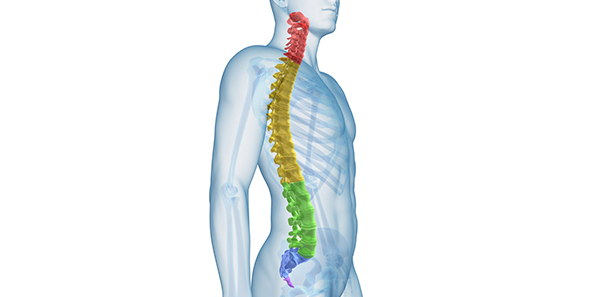
Classification
Depending on severity and the limitations imposed on the patient, effort angina can be divided into four levels.
- Class I: ordinary physical activity does not cause angina. Strenuous or rapid or prolonged physical activity provokes angina.
- Class II: there is some limitation of ordinary physical activity. Angina is provoked by walking or climbing stairs rapidly or by walking uphill.
- Class III: there is marked limitation of ordinary physical activity. There is angina pain on walking one or two blocks on the level or one flight of stairs at normal pace.
- Class IV: the person is severely disabled by angina and unable to carry out any physical activity without discomfort.
Examinations
- Electrocardiogram: approximately 50% of patients with angina have a normal ECG (electrocardiogram) when at rest and in the absence of pain, so a normal baseline ECG will not rule out coronary disease.
- Cardiac stress test: studies the clinical and electrocardiographic response to programmed physical exercise. Measures pain and changes in the ECG during physical exercise.
- Radioisotopic studies: simultaneous use of isotope contrast gammagraphy and the cardiac effort test.
- Echocardiogram: a bloodless way of assessing the motility – movement – of the various segments of the heart. It can be combined with the cardiac effort test or with administering pharmaceutical drugs in order to diagnose myocardial ischemia (stress echocardiogram).
- Cardiac catheterization (Coronariography): consists of inserting catheters into the arterial or venous system via percutaneous puncture, usually in the femoral blood vessels and under local anaesthetic. Other entry routes are the humeral or radial artery. From the entry point, the catheters are moved towards the heart and a contrasting fluid is injected, turning the heart structures opaque so they can be examined (angiography).
Treatment
The main aims of treatment are to improve patient prognosis, halt the advance of the coronary atherosclerosis, improve quality of life and prevent angina episodes.
The first step should be to monitor risk factors, control blood sugar levels, blood pressure and cholesterol. The patient should be placed on a heart-healthy diet (reducing the amount of saturated fat they eat and increasing their intake of legumes, fruit, vegetables and fish). They should be encouraged to take regular exercise, usually walking for around 4 kilometres every day. Patients with mild symptoms can play sport, provided they do NOT play competitively and do not experience discomfort.
1. Pharmacological treatment
The treatment of choice for angina crises is sublingual nitroglycerin, in either tablet or aerosol form. Nitrites reduce the oxygen consumption of heart muscle and dilate the coronary arteries. It should be administered as soon as the pain appears.
The only treatment that improves the prognosis of patients with stable coronary disease is the correction of coronary risk factors, preventing coronary thrombosis with plaque dissolving medication, administering medication that blocks or slows heart rate down (beta blockers) in patients who have had a recent heart attack, and certain blood pressure controlling pharmaceutical drugs. Junior aspirin reduces death and myocardial infarction (heart attack) rates by 30%.
2. Myocardial revascularization
In patients where medical treatments have proved ineffective or for people who feel that the quality of life that treatments gives them is unacceptable, myocardial revascularization by means of percutaneous coronary angioplasty or by surgery to graft a vein or artery is usually successful in eliminating angina crises and simplify medication.
- Transluminal percutaneous coronary angioplasty. Cardiac catheterization: consists of dilating the atherosclerotic lesion that obstructs the free flow of blood through the coronary artery by inserting a catheter with a balloon that inflates at high pressure. The procedure is usually completed by implanting a coronary stent.
- Surgical treatment. Consists of opening up a connection between the aorta and the obstructed coronary artery, bypassing the blockage that caused the lesion (aortocoronary bypass graft). A section of saphenous vein (from the leg) or from the internal mammary artery (internal thoracic artery) is used.
The choice of revascularization method used depends on the type of lesion, its location, the diameter of the coronary arteries affected and the patient’s clinical circumstances.
Dr. Juan Antonio Andreo Ramírez – ASSSA Medical Manager
The information published in this media neither substitutes nor complements in any way the direct supervision of a doctor, his diagnosis or the treatment that he may prescribe. It should also not be used for self-diagnosis.
The exclusive responsibility for the use of this service lies with the reader.
ASSSA advises you to always consult your doctor about any issue concerning your health.